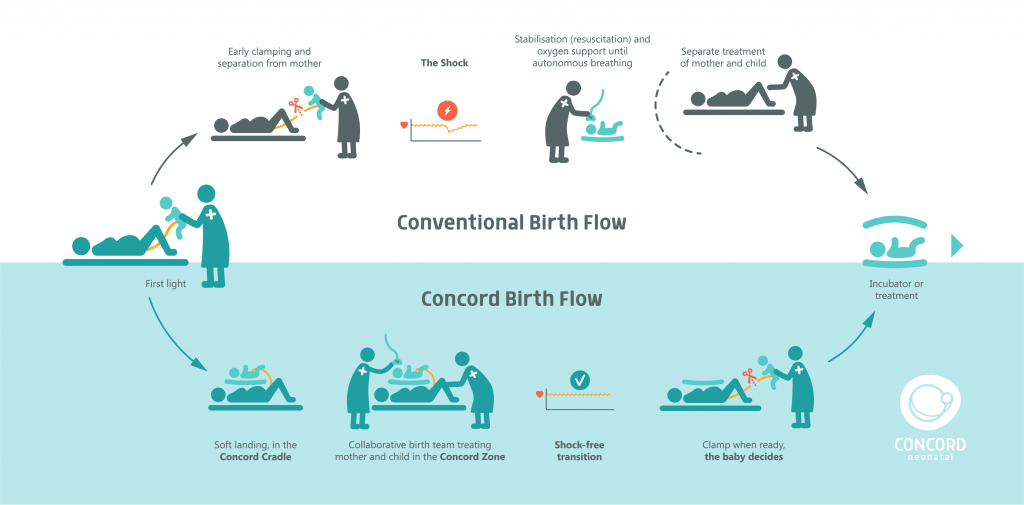
Start-up introduces new solution to enable caregivers to provide care, close to the mother, with the umbilical cord still intact
For babies who are born healthy, the World Health Organisation (WHO) recommends to delay cord clamping . It means that the umbilical cord is not clamped immediately after birth but after waiting one to three minutes. That way, the baby is still connected to the placenta and receives oxygen rich blood and essential nutrients.
However, ill or preterm born babies often require immediate care and are therefore removed from the mother. This is where Concord Neonatal, a start-up from the Netherlands, come into play: they just introduced a new solution, Concord, that enables caregivers to provide care immediately after birth with the umbilical cord still intact until the baby is stable and breathing on its own. To find out more, we interviewed Rianne Rotink, CEO of Concord Neonatal.
What is the idea behind Concord Neonatal and what was the starting point?
Professor Arjan te Pas and Professor Stuart Hooper have been studying the physiology of fetal to neonatal transition for many years, especially focusing on umbilical cord clamping. Studies with preterm lambs have shown that clamping the umbilical cord before the lungs fill with air results in a dangerous drop in heart rate and blood oxygen levels, increasing the risk of injury to organs. These studies also show that blood flow is a lot more stable during birth when waiting to clamp the umbilical cord until after the lungs aerate and breathing is established. This is called physiological-based cord clamping [1].
The first ideas to develop a solution started in 2015, by a team from Leiden University Medical Center (LUMC). To allow wider implementation and larger multicentre clinical research, Concord Neonatal B.V. was founded in 2017 as a spin-off from LUMC, to bring the solution to the market.
How did you/your team put the idea into practice?
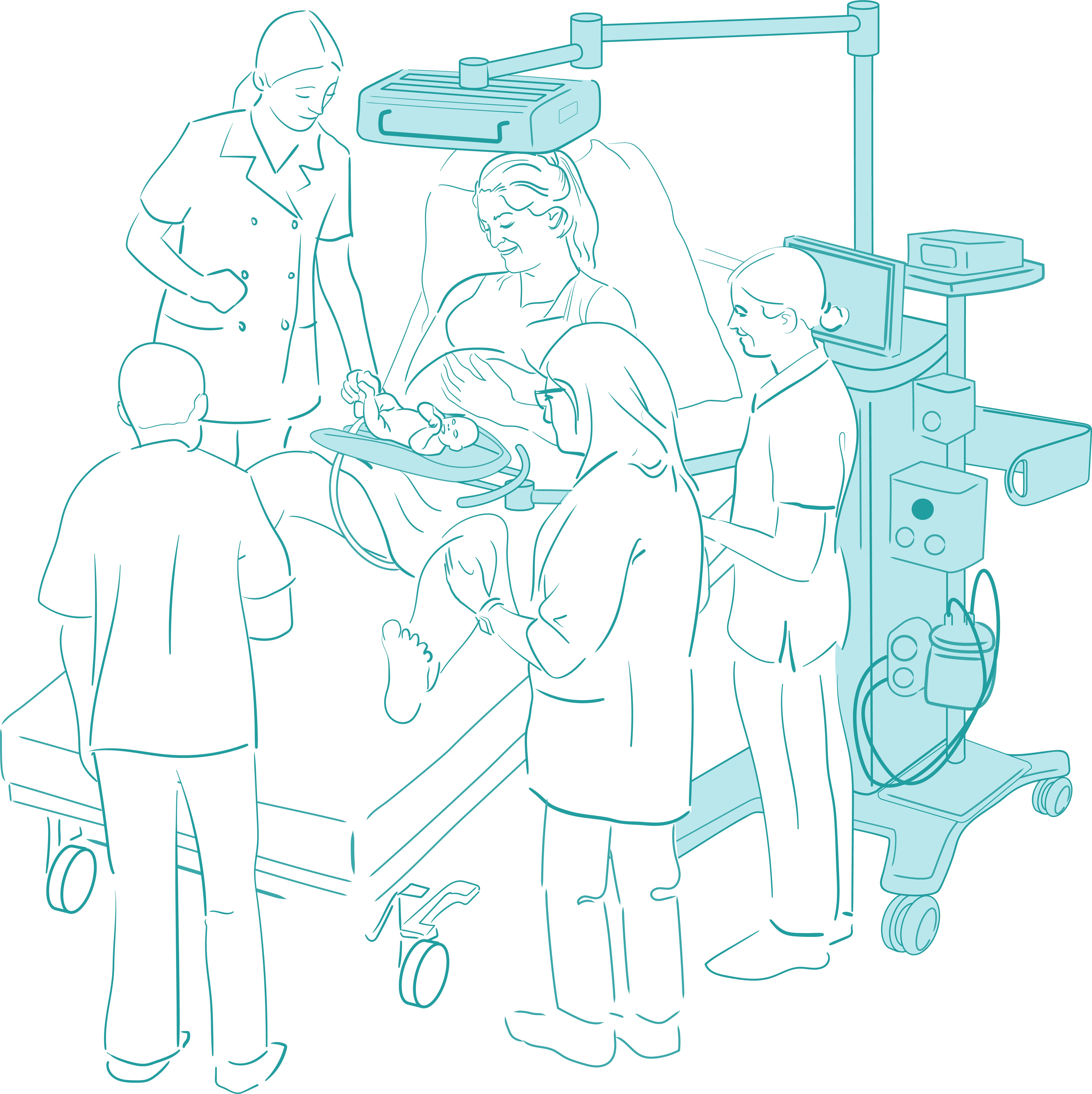
The team from LUMC developed a prototype of an innovative mobile trolley, called Concord, that creates a safe workplace for neonatal caregivers to provide lifesaving care with the umbilical cord intact. Concord Neonatal translated this prototype into a CE marked product and on March 7th, at the Dresden Symposium on Delivery Management, we proudly introduced the Concord Birth Trolley. Concord can be equipped with all necessary devices for adequate monitoring and treatment of newborn babies. There no longer is any urgency to cut the cord. All necessary care, without any compromise compared to the current standard care, can be provided immediately. The cord can later be clamped when the baby is fully stable and breathing on its own.
When is Concord used in neonatal practice, especially in the care of preterm or ill born babies? Please elaborate on the aspects which are particularly visionary in terms of delayed umbilical cord clamping as recommended by the WHO for improved maternal and infant health and nutrition outcomes.
WHO recommends to clamp the cord one to three minutes after birth (link). Unfortunately, it has not been possible for many hospitals to wait in case the baby needs urgent care. Due to lacking infrastructure they cannot offer adequate care with the umbilical cord still intact.
The Concord Birth Trolley enables hospitals to provide adequate newborn resuscitation without cutting the umbilical cord. This is applicable for all newborns who do not breathe or breathe insufficiently at birth and require breathing support or resuscitation. The majority of these babies are born preterm, but it is expected to also be beneficial for others, for example babies born with congenital diaphragmatic hernia or asphyxiated babies. Further research is planned to confirm this.
Which stakeholders did you involve in the development process (e.g. mothers, hospital staff)?
Concord was developed by a multidisciplinary team at LUMC consisting of neonatologists, obstetricians, Obstetric & Gynaecology (O&G) nurses, neonatology nurses and hospital engineers. Regular simulation sessions were done to test and refine the care protocol and the product, to ensure that obstetric and neonatal caregivers around the delivery bed can collaborate to provide the best care for mother and baby.
Which challenges did you face during the planning process of Concord Neonatal?
The main challenge for adoption of physiological-based cord clamping will be to adapt the caregivers’ workflow. Although the same care is provided, it is done in a different place, where collaboration between obstetrics and neonatology teams is essential. Clinical evidence is going to play an important role to show caregivers what the outcome improvement can be.
Which changes did you achieve and are there any measurable outcomes?
With a Concord prototype, made by LUMC, two clinical studies have been completed; ABC-1 in 2017 [2] and ABC-2 in 2018 (pending publication). ABC stands for Aeration, Breathing, then Clamping.
Until today, around 50 preterm infants have received a Concord birth.
A first study (ABC-1) to research physiological-based cord clamping took place. The outcomes of this study confirm what until now has only been confirmed in animal studies:
- The heart rate remained stable around the moment of clamping and no bradycardia was observed after;
- Oxygen levels in the blood (SpO2) increased at a faster pace compared to preterm infants receiving early cord clamping;
- The duration of hypoxemia was shorter in the first 10 min.
Avoiding hypoxemia, especially in the first minutes after birth, is pivotal since hypoxemia is associated with an increased risk of brain haemorrhage and death. With the realization of the Concord Birth Trolley, we are very proud to further investigate the improved outcomes of physiological-based cord clamping compared to time-based cord clamping (60sec). For the next study, we will use a multicentre randomized controlled trial as well.
You call Concord “not only a device, but a new care concept” and “baby-centred cord clamping”. Can you elaborate on this in more detail?
We call it baby-centred, since physiological-based cord clamping uses the baby’s condition to decide on the timing of cord clamping. We are therefore taking cord clamping, which today is regarded to be based on a set time (time-based cord clamping), one step further. Physiological-based cord clamping is a new way of working for neonatal and obstetric caregivers. We therefore call this a new care concept. Concord Neonatal wants to support hospitals in making this change, by not only providing the Concord Birth Trolley, but also to support hospitals in changing their way of working. We provide team workflow training to familiarize all caregivers with the new Concord Birth Flow to improve outcomes for babies who have a more difficult start in life.
View more:
- Concord Neonatal Website: https://concordneonatal.com/
- WHO guideline umbilical cord clamping
- WHO recommendations on optimal timing cord clamping
[1] Bhatt S, Alison BJ, Wallace EM, Crossley KJ, Gill AW, Kluckow M, et al. Delaying cord clamping until ventilation onset improves cardiovascular function at birth in preterm lambs. J Physiol 2013 Apr 15;591(Pt 8): 2113-26.
Hooper SB, Kitchen MJ, Polglase GR, Roehr CC, Te Pas AB. The physiology of neonatal resuscitation. Curr Opin Pediatr. 2018 Apr;30(2):187-191. doi: 10.1097/MOP.0000000000000590.
Hooper SB, Te Pas AB, Lang J, van Vonderen JJ, Roehr CC, Kluckow M, Gill AW, Wallace EM, Polglase GR. Cardiovascular transition at birth: a physiological sequence. Pediatr Res. 2015 May;77(5):608-14. doi: 10.1038/pr.2015.21.
[2] Brouwer E, Knol R, Vernooij ASN, et al. Arch Dis Child Fetal Neonatal Ed. doi:10.1136/archdischild-2018-315483